 Treatment of inflammation of the Uterus is prescribed according to its cause. If the inflammation is caused by a chill or exposure to cold during menstruation, the patient should start the treatment with a hot leg bath. However, a hot hipbath may replace this after two or three days. In case of pain, hot and cold hipbaths will be beneficial. The water should be altered from hot to cold, every two minutes and this should be repeated thrice.
Treatment of inflammation of the Uterus is prescribed according to its cause. If the inflammation is caused by a chill or exposure to cold during menstruation, the patient should start the treatment with a hot leg bath. However, a hot hipbath may replace this after two or three days. In case of pain, hot and cold hipbaths will be beneficial. The water should be altered from hot to cold, every two minutes and this should be repeated thrice.
As this disease produces the tendency towards constipation, the patient should take an enema once daily with warm water as can be comfortably borne by the patient. It is also desirable to apply alternate compress on the abdomen just before employing enema. In the chronic form the treatment should endeavor at increasing the general vitality. To begin with, the patient should opt to fasting on orange juice and water for two or three days. The procedure is to take every two hours from 8 a.m. to 8 p.m. the juice of an orange diluted with warm water on 50:50 ratio. If the orange juice does not agree, juices of vegetables such as carrots and cucumbers may also be taken. A warm water enema may be taken each day while fasting to cleanse the bowels.
The patient should also undertake moderate exercise and walking in the fresh air as it will help increase general health and vitality. According to ayurveda medicine, endometriosis is attributed to a vata imbalance caused by a buildup of ama. In order to correct this imbalance, a regular daily routine is suggested as part of treatment of inflammation of the Uterus. This includes moderating the workload and practicing meditation and yoga, as well as increasing rest and sleep.
The diet for the treatment of inflammation of the Uterus should include a little more oil, sweet foods (but not refined sugars), as well as some salt and warm foods such as cereal and stews. Also, plenty of warm to hot water should be consumed, while the consumption of foods such as meat, cheese, caffeine and alcohol should be minimised. Taking a laxative or 4 to 5 teaspoons of castor oil or senna tea are recommended on days 14 to 15 of your menstrual cycle, along with a light diet, in order for the treatment of inflammation of the Uterus.
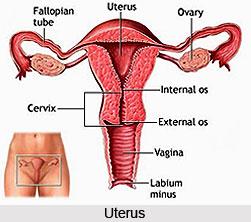
In order to prevent inflammation of the Uterus, activities should be minimised during days 1 to 3 of the menstrual cycle, and gentle exercises such as walking should be conducted instead of more vigorous activities like aerobics. The medical treatment of inflammation of the Uterus s is aimed at controlling the pain and shrinking of the endometrial tissue. A total hysterectomy, which is the removal of the uterus and the ovaries, is considered to be the only definitive cure for this ailment. There are three broad treatment methods of inflammation of the Uterus, namely treatment with drugs, treatment with surgery, and combination of drugs and surgery.
Drug or hormonal therapy aims at suppressing the activity of ovaries and slowing the growth of endometrial tissue. Some doctors recommend the long-term use of low-estrogen, high-progestin birth control pills unless a woman is trying to conceive. This form of treatment tends to lighten or even stop menstruation, which keeps the stray endometrial tissue from growing. Of the drugs used for the treatment of inflammation of the Uterus, birth control pills however have the mildest side effects.
Another hormonal treatment of inflammation of the Uterus is to suppress the body`s production of estrogen. There are a number of drugs in this category and they usually work by reducing or stopping the production of Follicle Stimulating Hormone (FSH) and Leutenizing Hormone (LH). One such drug is called Danazol, which is a powerful drug with actions similar to that of the hormone Testosterone. It works by reducing FSH and LH levels and is taken for six to nine months at a time.
Danazol has proved to improve symptoms and shrink the size of the implants for 89% of the women who consume it. However, women who use it may have severe side effects including pseudo-menopause, hot flashes, joint pain, vaginal dryness, muscle cramps, depression, weight gain, irritability, and acne. In extreme cases, there is masculinisation, which manifests as voice changes, reduction in breast size and overgrowth of body hair. Besides, about 30% of women treated with Danazol experience infertility later on and for those who conceive, there is a high risk of recurring pain after pregnancy. Because of its many side effects, Danazol is hardly used anymore.
The most commonly used hormonal drugs for the treatment of inflammation of the Uterus are called Gondotropin-releasing hormone agonists (GnRHa). These are derived from Gonadotropin-releasing Hormone (GnRH) which is a hormone secreted by the pituitary gland. These drugs stop the production of FSH and LH by overloading the pituitary`s production facilities. In effect, the GnRH analogs put an end to ovulation without eliminating the ovaries. As a result, just before the menopausal state characterised by an absence of menstruation and a significant reduction in estrogen levels, which in turn stops the endometrial growths and reduces the pain of inflammation of the Uterus. Side effects include hot flashes, mood swings, vaginal dryness, and calcium loss from bone. The side effects are stopped if one stop to take these medication and fertility is regained.
Another GnRH-a used in the treatment of inflammation of the Uterus is Leuprolide, which is administered as an injectable drug called Lupron or monthly implants beneath the skin called Zoladex. The mechanism of action and the side effects are the same as that of Nafarelin. Treatment with Lupron comprises one injection a month for six months. In clinical studies, the effectiveness of Lupron can also be compared to Danazol without all the potential side effects. In addition to hormonal drugs, painkillers are commonly suggested. These are non-steroidal anti-inflammatory drugs (NSAIDs) and include Naprosyn, Ponstel, Rufen, Meclomen, Motrin and others. In cases of severe pain, narcotic drugs like Codeine, Oxycodone, or even Morphine may be prescribed.
When there is moderate to severe inflammation of the Uterus, drug therapy will not be sufficient to ease the symptoms and surgery may be necessary. General surgery is needed when patches of endometrial tissue are larger than 1.5-2.0 inches, when there are noteworthy adhesions in the lower abdomen or pelvis, for endometrial growths that are obstructing one or both fallopian tubes, or when the pain is severe and not lessened by drug therapy. Often the tissues are removed during laparoscopy when the definitive diagnosis is made.
Laparoscopy is a minor surgical procedure done under anesthesia in which the patient`s abdomen is distended with carbon dioxide gas to make the organs easier to see and a laparoscope (a tube with a light at the end) is inserted through a tiny incision made on the abdomen. Laparoscopic surgery may involve burning of the tissue with electrical current, electrocautery, or laser to remove endometrial tissue. The advantage of this surgical approach, besides a shorter and less expensive hospital stay, include less chances of complications; abridged tissue injury, bleeding and blemish tissue formation; rapid diagnosis and treatment; and an easier, quicker and less painful recovery. It is an effective method of directly attacking the causes of pain and infertility, which are the main concerns of the sufferers. The potential side effects of laparoscopy are mainly associated with instrument insertion, heat injury, and potential painkilling complications.
Another surgical approach is Laparotomy; this procedure involves the opening up of the abdominal cavity and is considered major surgery. This is done when endometriosis is so extensive and perhaps accompanied by other interrelated diseases that it cannot be handled through the tiny slit used in laparoscopic surgery. For example, bladder, bowel and kidney involvement may need special surgical procedures only possible with Laparotomy. Also if there are very large cysts to be removed or large endometrial growths that form a mass involving a number of organs, Laparotomy is the only convenient method. There are a number of other operations and related tests that may need to be performed as part of the treatment for endometriosis, like Neurectomy, cutting or blocking the nerves that transmit the pain of endometriosis; Salpingectomy, removal of a fallopian tube; Intravenous pyelogram, an X-ray examination of kidney, bladder, and uterus using an injected dye; as well as several other methods to look for adhesions in colon, lungs and other areas.
The third approach in the treatment of inflammation of the Uterus is to use the combination of drugs and surgery. In this method, medicines are used for six weeks before the surgery to shrink endometrial tissue and ease the surgical removal. After the surgical removal, doctors may suggest a low dose estrogen-progestin birth control pill to be taken for up to nine months. Unfortunately, the relief of symptoms that follows surgery is often temporary. As a last resort of treatment, a total hysterectomy is performed that involves the removal of the uterus and both ovaries. Menopause also generally ends the action of mild to moderate inflammation of the Uterus.
The treatment of inflammation of the Uterus should be done under proper physician or specialist. The delicate reproductive system of women needs special attention, especially if it is a serious condition like inflammation of the Uterus.